Article Today, Hyderabad:
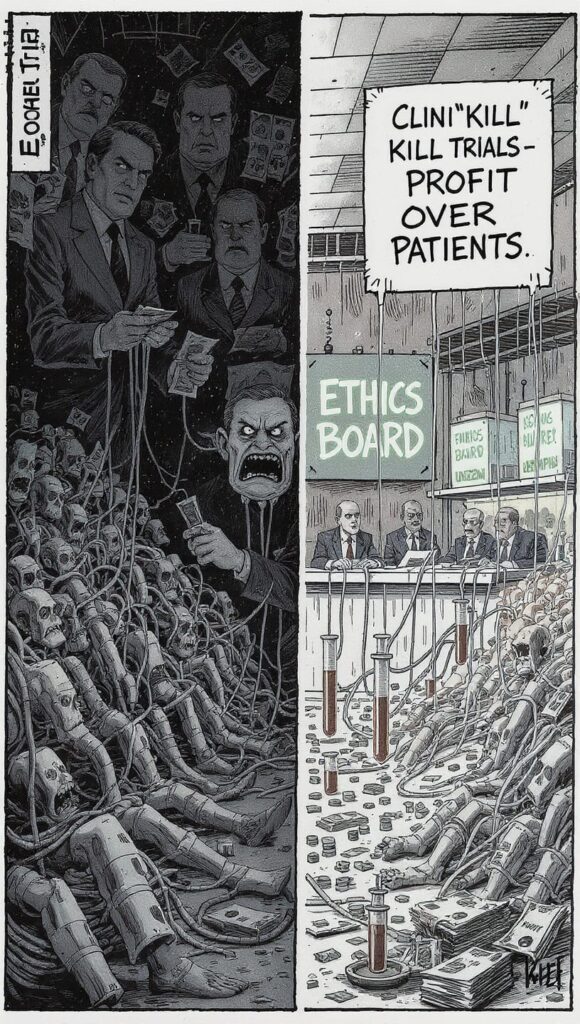
Concerns are mounting that clinical drug trials are increasingly compromising patient safety in the pursuit of profit. Experts fear that ethical review mechanisms, meant to protect participants, are losing their independence under the growing influence of private corporations. The controversy surrounding the diabetes drug Ozempic has reignited global debate over how far pharmaceutical companies can go in commercialising clinical research.
Private Control Over Ethical Oversight
Institutional Review Boards (IRBs), once independent guardians of patient welfare, are now being criticised for functioning as commercial entities. In the United States, several IRBs have come under private equity ownership, raising questions about transparency and accountability. For instance, Novo Nordisk selected WCG Clinical for its Ozempic (semaglutide) trials — a company financially linked to Novo Holdings. Reports indicate that the same company was chosen for at least 46 trials in the last six years, suggesting potential conflicts of interest. In India, similar patterns of close ties between pharmaceutical firms and local ethics committees have sparked alarm.
Profit Over Patient Protection
Traditionally, ethics committees operated within universities and hospitals on a non-profit basis. However, many have transformed into large commercial entities such as WCG and Advarra. These organisations now play active roles not only in reviewing but also in conducting trials, recruiting volunteers, and analysing data.
Their financial dependence on drug companies has raised fears that reviews are being compromised. Though the Central Drugs Standard Control Organisation (CDSCO) regulates trials in India, experts say independent ethical scrutiny remains weak, leaving room for undue corporate influence.
Weak Regulation and Transparency Gaps
Regulatory oversight of ethical review boards remains inadequate worldwide. Most IRBs are not legally required to disclose the quality or integrity of their reviews, making accountability difficult. In India, despite guidelines issued by the CDSCO and the Indian Council of Medical Research (ICMR), enforcement remains inconsistent. Reports continue to surface of trials being conducted without fully informed consent or adequate disclosure to participants, highlighting persistent gaps in compliance.
Repeated Ethical Lapses
Ethical violations in clinical research are not new. The 1972 Tuskegee Syphilis Study in the United States remains a stark reminder of what happens when oversight fails. In India, incidents in Hyderabad in 2005 revealed that patients had been enrolled in drug trials without complete consent. Although regulatory tightening followed in 2019, experts say implementation on the ground remains weak. As a result, public confidence in pharmaceutical research continues to erode.
Global Alarm Over Ozempic Trials
The ongoing controversy around Ozempic has intensified scrutiny of clinical testing practices. Reports suggest over 2,300 complaints have been filed globally, linking the drug to gastrointestinal and gallbladder complications. Analysts say these developments expose systemic flaws in how trials are monitored and reviewed. Unless stronger safeguards are enforced, experts warn, the line between scientific progress and human exploitation will continue to blur.



